What's the story with pelvic floor disorders?
Chances are if you talk to a friend – or a mother, an aunt, or a sister – you will discover you are not alone in having a symptoms of a pelvic floor disorder. In fact, 40-50% of women will have a pelvic floor disorder during their lifetime and 1 in 5 women will have surgery for a pelvic floor disorder such as vaginal prolapse in her lifetime. And while pelvic floor disorders are intimate and can be embarrassing to discuss, more women are feeling empowered to discuss their symptoms of pelvic floor disorders because there are options to treat their symtoms that can be life changing. With the abundance of TV and magazine advertising, certainly urinary incontinence is now being discussed more than ever before. While pelvic floor disorders are not life-threatening, but they have a big impact on quality-of-life.
 What is a pelvic floor?
What is a pelvic floor?
What is a pelvic floor disorder?
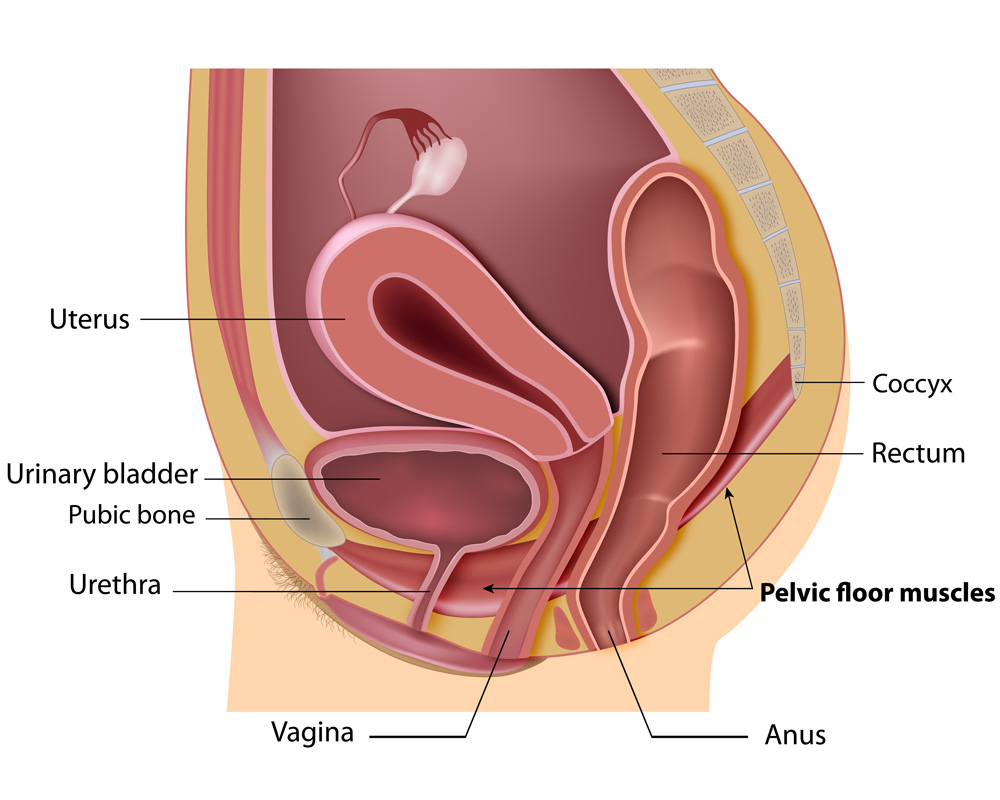
Definitions are important so I first want to define what is the pelvic floor and what is a pelvic floor disorder. The pelvic floor is the support for the pelvic organs – such as the vagina, uterus, rectum/bowel and urethra and bladder. The pelvic floor is made up of muscles and ligaments that attach to the bony pelvis for support. If there is weakness or disruption of these support structures, it can result in experiencing symptoms such as urinary leakage, accidental bowel leakage, and/or vaginal bulge symptoms from uterine or vaginal prolapse.
Main types of pelvic floor disorders
Here are the four main disorders:
- Overactive bladder and urge urinary incontinence – bothersome frequent urination, sudden urinary urgency and leakage before making it to the bathroom
- Stress urinary incontinence – leakage with activity such as running, coughing, laughing, jumping
- Fecal incontinence – leakage of stool beyond one’s own control
- Vaginal prolapse – loss of support of one or more areas of the vagina such that the walls of the vagina start to come down to or outside the vaginal opening. This can include:
a. Cystocele: loss of support of the anterior vaginal wall that supports the bladder
This can cause a sense of difficulty emptying the bladder or trying to urinate
b. Rectocele: loss of support of the posterior vaginal wall that supports the rectum
This can cause a sense of stool getting stuck or blocked when trying to have a bowel movement
c. Uterine prolapse: loss of support of the uterus and cervix so the uterus falls down toward the opening or outside the vagina.
d. Vaginal vault prolapse: if you have had a hysterectomy the top of the vagina can fall toward the opening or outside the vagina where the uterus used to be.
How can you tell if you have a pelvic floor disorder?
If you are suffering from a pelvic floor disorder maybe you are noticing changes such as:
- Constant awareness of bathroom locations
- Reducing intake of fluids
- Changing level of activity to lessen symptoms of leakage or vaginal bulge symptoms that may worsen with strenuous activity
- Having a spare pair of clothes in the car
- Avoiding going out of the house because of fear of having an accident
- The constant feeling of a stuck tampon because the vagina is prolapsing toward the outside
These are common changes and symptoms of women with pelvic floor disorders
Talk to us! We are not embarrassed by pelvic floor disorders!
I have some patients who come in and say they feel embarrassed to be talking about these issues, but we want you to know – taking care of pelvic floor disorders is what we do and we talk about it all day long! We hope to help you feel at ease knowing you are not alone. Lets talk about it and make your life better!
Minnesota Women’s Care was founded by Dr. Melvin Ashford – a trained Urogynecologist (also called Female Pelvic Medicine and Reconstructive Surgeons), who can help you with these bothersome pelvic floor disorders and educate you about your pelvic floor disorder and treatment options. There are non-surgical and surgical treatment options. A lot of factors go into what treatment is best for you. This can include prior treatments, desire for more children, level of activity and other medical conditions. We believe in shared patient decision making here at Minnesota Women’s Care and we hope you will leave your visit feeling informed and empowered to make some changes to improve your quality-of-life.
